
You can get more credit towards higher levels of medical decision making (MDM) using 2021 E/M data guidelines that allow you to give more points for tests that your provider orders and/or reviews. The money is just waiting for you to take it.
Getting paid accurately for your office visits in 2021 hinges on your ability to correctly count the amount of data involved in a service. The new E/M guidelines have massive changes that you MUST master now to avoid leaving dollars on the table – or huge paybacks and penalties.
The 2021 E/M MDM rules for scoring the data category are deceptively simple; there are several gray areas that can trip you up – and land you with too much or too little pay – unless you know how to correctly apply the guidelines …
How to Score MDM Data Per 2021 E/M Guidelines
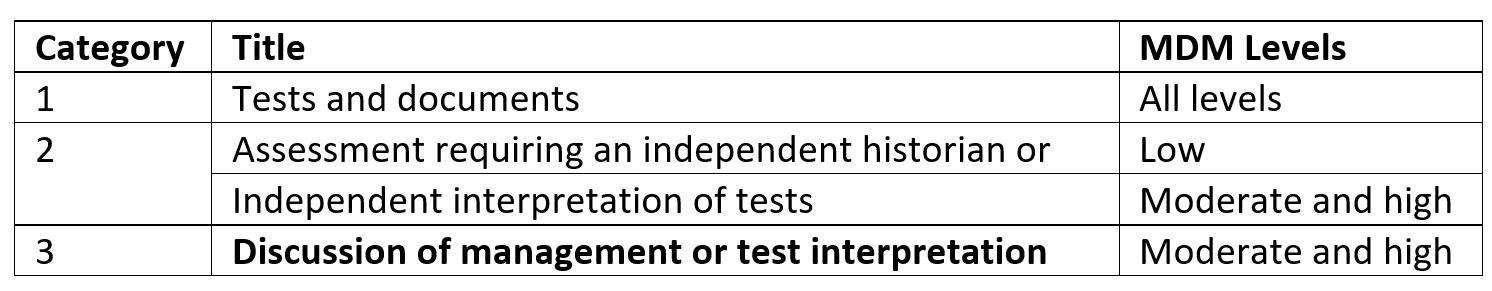
Out of the three elements of MDM, element #2 for the “Amount and/or Complexity of Data to be Reviewed and Analyzed” has the most new 2021 rules as compared to your old and familiar 1995/1997 guidelines. The new element contains:
Give One Point Per Test Modality
You should assign points for ordering and reviewing data for “each unique test,” according to the 2021 E/M guidelines. Tests include:
- Imaging
- Labs
- Psychologic data
- Physiologic data
You’ve gotten added opportunities to score additional test points. The guidelines state that “the differentiation between single or multiple unique tests is defined in accordance with the CPT code set.”
Here’s how that could affect your scoring. Your physician orders an X-ray and an MRI for a patient.
Old way: According to the 1995/1997 guidelines, you would assign only one point, because these tests are the same modality — both fall under the radiology section of the CPT code set (70010-79999).
Change: In 2021, you’d get two points, because the x-ray and MRI are two different tests (although the modality is the same).
A panel of tests is considered as one unique test. The 2021 guidelines give the example of “basic metabolic panel” (80047). Although the panel contains several tests, they are encompassed under one CPT code.
Ordering a Test is Credited Separately from Reviewing that Test
A big change in the 2021 E/M guidelines is that you can give the provider credit for both ordering and reviewing the same test. The 1995/1997 E/M guidelines credited both pieces together. The credit hinges on the review date. Assign the point based on these scenarios:
- Same session results: Provider orders and performs the lab in-house and has the results before the patient leaves. Do not give credit for the order or review.
- Different day results provided with no subsequent encounter. A patient’s labs come back a couple days after the visit, and the physician calls the patient to discuss the results. The provider prescribes a medication and amends the documentation for the E/M visit to include review of the test results. You should give the provider credit for both ordering and reviewing the test on that same visit.
- Different encounter for results review: A provider orders the test, receives the results after the visit, and then schedules a follow-up visit with the patient in which the test results are reviewed and discussed. Should you count the review of the test results at the first encounter when you’re documenting the discussion of the results at the subsequent encounter? Not all experts agree.
- CPT language: “Ordering a test is including in the category of test result(s) and the review of the test result is part of the encounter and not a subsequent encounter,” according to the 2021 E/M guidelines. Based on this language, some experts advise you’d credit both ordering and reviewing at the initial visit. In other words, it’s assumed that if a provider orders a test, he or she intends to review it eventually.
- Confusion: Other experts say the review should be credited on the subsequent visit, because the notes for that visit will indicate the review and discussion.
- Do this: This is a gray area, and perhaps AMA, CMS, and payers will offer clarifications in 2021. In the meantime, your practice should decide on one interpretation or the other, document that interpretation in your policies and procedures, and have all providers abide by that policy. If CPT or CMS does eventually provide a clear interpretation, amend your policy.
E/M Related to CPT and E/M Coding Related
 |
 |
 |
||||||||
| . | ||||||||||
| Master Massive E/M Coding Changes (99201-99215) by Jan. 1 Deadline |
Get More E/M Money with New 2021 Medical Decision-Making Rules |
Get Paid $25/ea. for New Patient COVID-19 Testing With 99211 |
||||||||
|
|
|
